this post was submitted on 07 Oct 2024
1918 points (99.3% liked)
Microblog Memes
6024 readers
2502 users here now
A place to share screenshots of Microblog posts, whether from Mastodon, tumblr, ~~Twitter~~ X, KBin, Threads or elsewhere.
Created as an evolution of White People Twitter and other tweet-capture subreddits.
Rules:
- Please put at least one word relevant to the post in the post title.
- Be nice.
- No advertising, brand promotion or guerilla marketing.
- Posters are encouraged to link to the toot or tweet etc in the description of posts.
Related communities:
founded 1 year ago
MODERATORS
you are viewing a single comment's thread
view the rest of the comments
view the rest of the comments
Had my buddy over who brought over his incredibly questionable 30yo brother who shared some real incel levels of talk. He used my bathroom and asked if I wore tampons since a pack was visible. Like bro, I have a wife and a daughter.
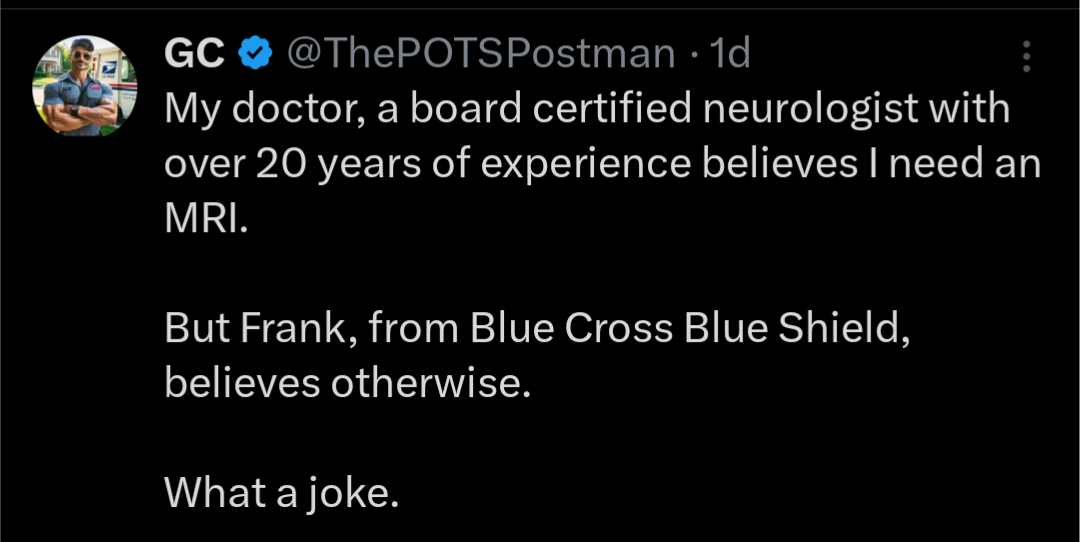
Anyways, that guy works in health insurance!
I don't know how much decisions he can actually make. But that dude has a middle-school level education about sex ed and struggled to explain what a period is. And he is one of the barriers to approving/rejecting your health care.
“You want me to whip out my dick and slap you with it since that was the stupidest question I’ve heard?”
You should see what @pancakes@sh.itjust.works wrote in this very thread. You basically just answered their question about what this industry must do to a person's ability to empathize and be a decent person to others. Or in this case, maybe lack thereof is a job requirement?
There's different teams doing different types of work.
Like the claim system might have it setup so X codes in Y situations can't be automated. Then someone looks at the claim, determines based on their written guidelines that this one needs to be reviewed so they look to see if there are notes attached. If there aren't they request the notes, maybe by sending a letter. If there are, they send it to the team that reviews notes and makes these decisions. Those people probably also have written guidelines on what is allowed or not and if it's more complicated they (should) have someone qualified that can review it. Then the claim is probably sent back to the other team saying "Hey, deny that code and allow this code", where they then just do whatever that says.
They probably also have situations where X code in Y situation is "never" allowed and the first people reviewing it just always deny it. Then, as mentioned elsewhere here, the provider has to resubmit it and then it's allowed on "appeal" by another team. This brother you mentioned is probably doing very little decision making beyond applying already decided guidelines to each claim, if he even processes them.